INTRA AND INTERTESTER RELIABILITY AND THE EFFECT OF SEVERAL REPETITIONS ON PAIN AND RESISTANCE
A cura di: Carla Vanti, Laura Conteddu, Andrew Guccione, Filomena Morsillo, Sergio Parazza, Carlotta Viti e Paolo Pillastrini.
Vai all’articolo in versione PDF: ULNT Intra e inter reliability.
Abstract
Objective: The aim of this study is to measure the intra- and intertester reliability of the Upper Limb Neurodynamic Test 1 in asymptomatic subjects with respect to onset of pain, submaximal pain (SP), first resistance (R1), and second resistance, and determine the effect of several repetitions of the test.
Methods: Three physiotherapists evaluated the dominant upper arm of 36 asymptomatic adult subjects 5 times with
an electrogoniometer.
Results: Intratester reliability for R1 was good with an intraclass correlation coefficient (ICC 3,1) ranging from 0.69 to 0.91. Intertester reliability was fair for R1 (0.48, standard error [SE] = 0.14), second resistance (0.62, SE = 0.011), and SP (0.64, SE = 0.09), but good for onset of pain (0.72, SE = 0.011). The ICCs on 5 repetitions for each observer were higher, ranging from 0.51 (R1, SE = 0.066) to 0.76 (SP, SE = 0.049). Using the data from the 2 more expert physiotherapists, almost all ICCs were in the good range. The effect of 5 repetitions was a statistically significant progressive improvement of range on all parameters from the first to the final repetition.
Conclusions: Our results regarding the reliability are in line with other studies on the reliability of manual therapy tests. Moreover, the cumulative effect of repetition suggests that the Upper Limb Neurodynamic Test 1 may warrant investigation as a treatment technique. (J Manipulative Physiol Ther 2010;33:292-299).
Key Indexing Terms: Reproducibility of Results; Neurologic Examination; Upper Extremity; Median Nerve.
People and place
- Lecturer of Manual Therapy Sciences, School of Physiotherapy, University of Bologna, Bologna, Italy and Private Practice, Castenaso, Bologna, Italy.
- Private Practice, Castenaso, Bologna, Italy.
- Deputy Director, Health Services Research and Development Service, Department of Veterans Affairs, Washington, DC, United States.
- Regional Health and Social Agency, Region Emilia-Romagna, Bologna, Italy.
- Private Practice, Castenaso, Bologna, Italy.
- Private Practice, Castenaso, Bologna, Italy.
- Associate Professor of Rehabilitative Sciences, Dipartimento di Medicina Interna, dell’Invecchiamento e Malattie Nefrologiche, Occupational Medicine Unit, S Orsola–Malpighi Hospital, School of Physiotherapy, Alma Mater Studiorum, University of Bologna, Italy.
Submit requests for reprints to: Carla Vanti, PT, Studio Privato di Fisioterapia, Via Tosarelli 144 40055 Castenaso, Bologna, Italy (e-mails: cavanti@tin.it, lauraconteddu@gmail.com, andrewguccione@cox.net, filomena.morsillo@unibo.it, s.parazza@alice.it, cviti.fisio@gmail.com, paolo.pillastrini@unibo.it).
Paper submitted July 6, 2009; in revised form December 7, 2009; accepted December 29, 2009.
0161-4754/$36.00 Copyright © 2010 by National University of Health Sciences.
doi:10.1016/j.jmpt.2010.03.003
Mechanical forces and mechanosensitivity of the nervous system
Research interest in the relationship of mechanical forces and mechanosensitivity of the nervous system and musculoskeletal disorders is increasing.(1,2) When physical capability of the nervous system is challenged by mechanical forces beyond its threshold of tolerance, a peripheral neuropathic condition, such as nerve root or peripheral nerve trunk injuries as well as radiculopathies and nerve entrapments, may ensue.(3) Furthermore, these challenges to the nervous system may contribute to the development of other painful conditions or syndromes such as lateral epicondylalgia, Achilles tendinosis, heel pain, and ankle sprains.(4) Signs and symptoms such as pain, dysesthesia, paresthesia, muscular spasm, or signs of a reduced nerve impulse conduction (weakness, anesthesia, hypoesthesia) on clinical examination contribute to the diagnosis of these conditions and further implicate the nervous system as the locus of the problem.(5) If the nervous system has increased mechanosensitivity, it can be demonstrated on neurologic and neurodynamic assessment.(6-8)
“Neural tissue provocation” or “neurodynamic” tests “challenge the physical capabilities of the nervous system by using multijoint movements of the limbs and/or trunk to alter the length and dimensions of the nerve bed surrounding corresponding neural structures”.
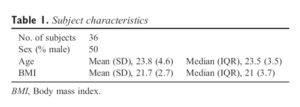
Tab.1 Subject characteristics
(4) The Upper Limb Neurodynamic Tests (ULNTs), as described by Butler, which are also called Upper Limb Tension Tests (ULTTs) or Upper Limb Neural Tension Tests, move the neural tissues and stimulate them mechanically, and provide insight into the mobility of the nerve structures and tissue sensitivity to mechanical stresses.(9) Among these Upper Limb Neural Tension Tests, the ULNT1 in particular accentuates the stress on the median nerve.(10-12) This test is performed by implementing different maneuvers in the following manner: while preventing elevation of the shoulder girdle, the shoulder is abducted and the wrist is extended; supination of the forearm is followed by lateral rotation of the shoulder and elbow extension. Although these tests are commonly used as part of clinical assessment,(13) few studies have investigated their intra- and intertester reliability and the effect of several repetitions with asymptomatic subjects. Hines et al (14) carried out an intertester reliability study looking only at the parameter “first resistance”, which is the minor resistance that an examiner first appreciates during a test such as a ULTT.(15) Using asymptomatic subjects who were examined by 4 different physiotherapists over 4 consecutive days, Hines et al concluded that there was a low intertester reliability of first resistance during the performance of ULTT. Byng (16) evaluated the intertester reliability of the ULTT performed by 2 physiotherapists on asymptomatic subjects using an apparatus to control the position of the subject’s head and shoulder, and no significant difference between examiners was found. Van der Heide et al (17) evaluated the intratester reliability of the Neural Tissue Provocation Test using an apparatus to maintain the position of the shoulder, wrist, and fingers. She concluded that the “first onset of pain” and the “increase of pain” were highly reliable findings when controlling the testing condition.
Similarly, Coppieters et al (18) found strong intra- and intertester reliability examining both symptomatic and asymptomatic subjects for the parameters “onset of pain” (OP) and “submaximal pain” (SP) measured within the same session, but also noted that reliability decreased when 48 hours between measurements had elapsed. They also varied their testing conditions across 3 different experiments, conducting the first two under laboratory conditions and the third in a clinical setting. Coppieters et al concluded that pain provocation during neurodynamic testing was a stable phenomenon and that the moments at which subjects complained of OP and SP during elbow extension could be reliably measured under both laboratory and clinical conditions.

Fig 1. The positioning of the electrogoniometer at the first stage of the ULNT1.
The aim of our study was to measure the intraand intertester reliability and clarify the effect of the repetitions of the ULNT1 on asymptomatic subjects, both for pain and resistance, using an electrogoniometer and without any external apparatus for maintaining or controlling the patient position to approximate how this test is typically performed in the clinic. Following some of the recommendations of Coppieters et al,18 it was decided to use a larger sample of asymptomatic subjects, a larger number of examiners, and a larger number of test repetitions.
METHODS
The study was approved by the Ethics Committee of the University Hospital S Orsola-Malpighi–Bologna (Italy) registration (no.4668).
Examiners
The intervention team was composed of 5 individuals: 3 experienced physiotherapists and 2 students. The physiotherapists, who were called Physio 1, Physio 2, and Physio 3 (with 8, 7, and 3 years of experience, respectively,in manual therapy), performed the ULNT1 (the “test”). The 2 students were at their final year of study at the School of Physiotherapy, University of Bologna, Italy; and their tasks were to set up the experiment and to record data.
Subjects
Forty-two asymptomatic right-handed subjects (ages, 19-41 years) were initially selected for the study. Inclusion criteria were asymptomatic adult individuals with full range of motion (ROM) of upper limb joints. Exclusion criteria were history of cervicobrachial pain on either arm or sign of local musculoskeletal dysfunction on the upper quadrant.
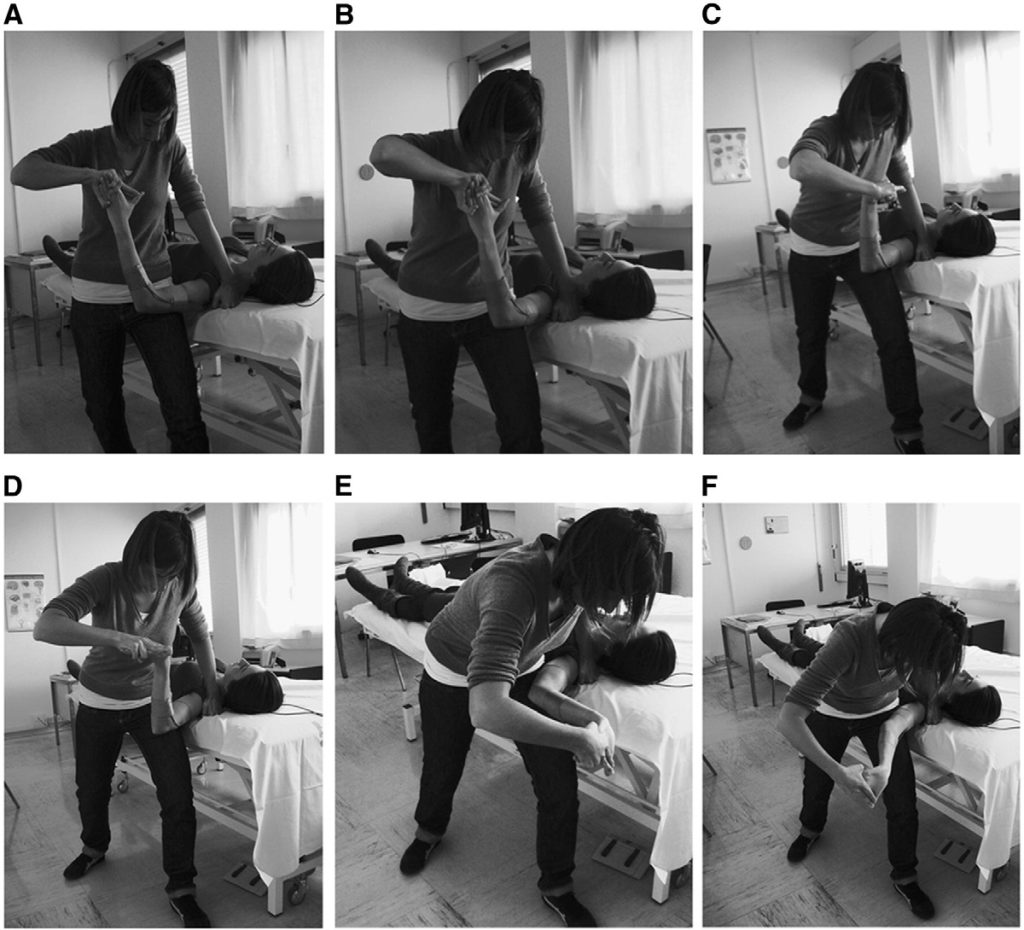
Fig 2. Stages of the ULNT1: (A) starting position; (B) shoulder abduction; (C) wrist extension; (D) forearm supination; (E) shoulder lateral rotation; and (F) elbow extension.
A questionnaire and a brief physical examination were performed as prescreenings to verify eligibility for the study according to our inclusion and exclusion criteria. All subjects signed an informed consent before commencement of the test. On the day of the test, 6 people dropped out citing personal reasons unrelated to the study, leaving a final sample 36 people, 18 male (median age, 22 years [interquartile range {IQR}, 3]) and 18 female (median age, 24 years [IQR, 5]) subjects. Demographic data are presented in Table 1.
Test Description and Procedure
In a preliminary meeting, the examiners compared their way of performing the test to try the best standardization of the maneuver (eg, strength, smoothness, rhythm) and to minimize potential sources of error during the performance of the test. Before the execution of the test, the subjects were informed regarding its characteristics. Subsequently, the subjects participated in a practice trial of the test using their left upper limbs, during which they had the opportunity to practice communicating their symptoms using standardized verbal signals. OP was defined as the moment when the first strain or discomfort was felt, whereas SP was defined as the strain becoming excessive or painful. The former was recorded by verbalizing Now, whereas the latter was recorded when the subject pronounced the word Ouch. Following Maitland,15 we evaluated both the first (R1) and the second (R2) resistance appreciated by the examiners. R1 is described as the point of the ROM “where minor resistance is first appreciated by the examiner”, 14 whereas R2 is the “location in range where maximum resistance is perceived by the therapist”.19 The former was recorded when the examiner pronounced the word R1, and the latter was recorded when the verbal signal R2 was uttered. The students who acted as data recorders noted the angular degree of the elbow for the 4 cited parameters using an electrogoniometer (Twin Axes SG110 with display unit ADU301, battery 9 V; Penny & Giles Biometrics Ltd, Gwent, United Kingdom); however, the examiners were blinded to the results. Flexible electrogoniometry as a measure of joint kinematics has been validated in several studies on the knee, (20-23) on the ankle, (24,25) and on the wrist.(26,27) The electrogoniometer we used has exhibited good reliability in evaluating joint movement and is preferable to the universal and fluid goniometer with respect to reducing intertester differences.
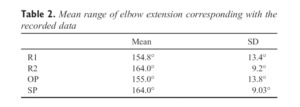
Table 2. Mean range of elbow extension corresponding with the recorded data
(28) Subjects were in supine position, without pillow, close to the border of a high/low plinth, with the lower limbs straight and the left upper armin neutral position.Afterward, a marker of adhesive tape was attached over the plinth as a reference point for a reliable positioning of the shoulder girdle. The axis arms of the electrogoniometer were positioned over the lateral side of the upper limbs (arm and forearm, respectively) after verification of the setting that was best suited to allowthe least possible soft tissue movements. The connecting cables from the axis arm to the display unit were positioned proximally (Fig 1), following the written instructions for the use of this device. Both electrogoniometer axis arms and connecting cables were attached to the upper limb by adhesive tape and foam underwrap. The electrogoniometer was reset before starting each session.
The ULNT1 was performed by the 3 physiotherapists as described by Butler.6 The shoulder girdle of the tested arm was stabilized in a neutral position without any external device to maintain or control it, after which the shoulder was abducted to 110°, the wrist and fingers were extended, the forearm was supinated, the shoulder was laterally rotated to 90°, and then finally the elbow was extended (Fig 2). If symptoms or second resistance were elicited, the test was stopped at SP and/or R2 points of range; if no symptoms or sensations were elicited, the test was done throughout the full available range. The 3 examiners performed 5 consecutive repetitions of the test. Between one tester and the following one, there was 1 minute of break to adapt the height of the plinth to each examiner. The order of entrance of the tester was randomized.
Statistical Analysis
All measurements were analyzed with respect to their normal distributions by skewness-kurtosis test. We used an intraclass correlation coefficient (ICC) to calculate reliability.
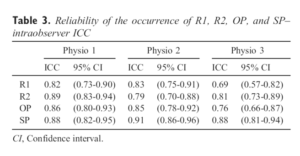
Table 3. Reliability of the occurrence of R1, R2, OP, and SP– intraobserver ICC
A linear model with random effects was fitted to estimate the ICC (3,1), which is appropriate to a linear model with random effects in which the subject has been defined as random effect to estimate the component of variance, whereas the observer is regarded as a fixed effect (the variance of the physiotherapist is included in residual variance). The model estimates the 2 variance components necessary to calculate the ICC, those assigned to the subject (a) and those due to the measurements on the same subject by 3 physiotherapists (b + c + d). The relationship between a and a + b + c + d is an estimate of the ICC. For the estimation of the interobserver ICC, separate models were estimated: the first one using data from the 5 repetitions of the 3 physiotherapists on 36 subjects and the other one using data on 5 repetitions but excluding one physiotherapist at a time, for pairwise comparisons. The standard error was estimated using the standard method. The same linear model with random effects was used to calculate the ICC interobserver for all possible observer pairs, using the data from the first repetition of each of the 3 observers. In this case, a bootstrapping technique was used to estimate standard error because the observations are less numerous. We calculated intraobserver reliability using 5 repetitions of the single observer. To obtain the intraobserver ICC, 3 separate models were estimated, one for each physiotherapist using data from the 5 repetitions performed on 36 subjects. The total variance of the measurements contains only the variance of individual measurements (d). Following Coppieters et al,18 we used the following criteria to judge the magnitude reliability coefficients: poor reliability = ICC less than 0.40; fair reliability = ICC at least 0.40 but less than 0.70; good reliability = ICC at least 0.70 but less than 0.90; and excellent reliability = ICC at least 0.90. The multivariate analysis of variance for repeated measurements of a “one-within” design was performed (using all 5 repeated measurements) to answer the question of whether there is change over time of ROM. For all analyses, the level of significance was set at P b .05; and the software used was STATA 9.0 SE (StataCorp LP, College Station, TX).
RESULTS
The mean range for R1 recorded in right dominant arm of the asymptomatic subjects was 154.8° (SD, ±13.4°),whereas for R2, it corresponded to 164.0° (SD, ±9.2°); the mean range of OP was 155.0° (SD, ±13.8°), whereas the mean range for SP was 164.0° (SD, ±9.03°) (Table 2).
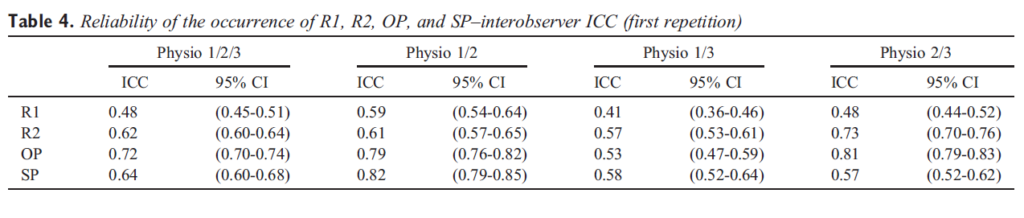
Table 4. Reliability of the occurrence of R1, R2, OP, and SP–interobserver ICC (first repetition)
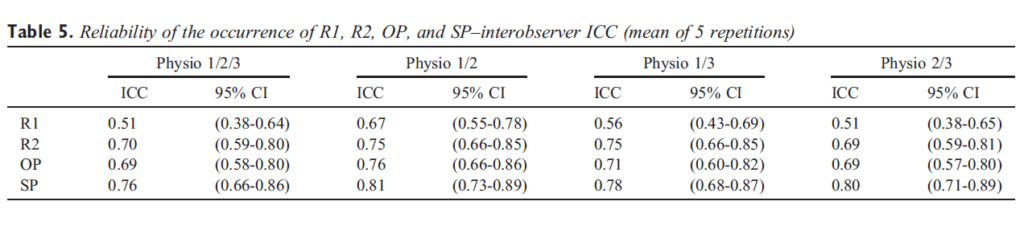
Table 5. Reliability of the occurrence of R1, R2, OP, and SP–interobserver ICC (mean of 5 repetitions)
There was a high degree of similitude between subject and examiner findings: in particular, considering the total number of 540 data points, both OP and R1 scores as well as SP and R2 scores are very similar to each other. The intratester reliability across all measures ranged from 0.69 to 0.91 (Table 3). Intratester reliability was higher for R2 than R1 and for SP than OP; moreover, the reliability was better for subjects’ self-reports (OP and SP) compared with professional judgments (R1 and R2). Overall, SP was the most reliable measurement; and R1 was the least reliable. For intertester reliability, the ICC (3,1) calculated using data from the first repetition of the ULNT1 for each of the 3 examiners (ie, Physio 1, Physio 2, and Physio 3) was only in the fair range for R1 (0.48, SE = 0.14), R2 (0.62, SE = 0.011), and SP (0.64, SE = 0.09), but was in the good range for OP (0.72, SE = 0.011) (Table 4). Furthermore, with respect to the intertester reliability between Physio 1 and Physio 2 (the more expert physiotherapists), the ICCs were in the “good” range for subject parameters (OP = 0.79, SE = 0.015; SP = 0.82, SE = 0.017). The ICCs calculated using 5 repetitions for each observer are higher, ranging from 0.51 (R1, SE = 0.066) to 0.76 (SP, SE = 0.049). Using the data from Physio 1 and Physio 2, almost all ICCs were in the “good” range (R1 = 0.67, SE = 0.058; R2 = 0.75, SE = 0.048; OP = 0.76, SE = 0.048; SP = 0.81, SE = 0.042) (Table 5). Similar to what we observed regarding intraexaminer reliability, the interexaminer reliability was higher for subjects’parameters (OP, SP) in comparison to raters’ parameters (R1, R2). Moreover, our data support an association between reliability and physiotherapists’ experience. To explore the effect of 5 repetitions of ULNT1 on mean elbow range, we considered the mean measurements of each repetition (first, second, third, fourth, and fifth) for all observers and found statistically significant improvement of range for all 4 parameters (R1, R2, OP, and SP) with each successive repetition (respectively, F(df 4, 475) = 8.04, F(df 4, 472) = 7.38, F(df 4, 444) = 14.03, and F(df 4, 351) = 7.53; P = .00). The proportionate increase from the first to the last repetition is similar for each one parameter and examiner (Fig 3).
To explore the effect of 15 repetitions, we used the median measurement of each repetition of each observer and found a positive effect of repetitions on the measurements after subtracting the “physiotherapist effect” (regression coefficient N0). When we subtracted the “physiotherapist effect,” whose coefficient is significantly negative, we observed a reduction on the irst measurement.In addition, we noticed different rates of increase among individuals, significant differences across the initial measurements of each of the 3 physiotherapists, and inverse relationship between the first measurement and the rate of increase; that is, subjects who started with a lower measurements showed a higher rate of increase (Fig 4).
DISCUSSION
This study is the first that considers both subject and examiner parameters, using a different number of repetitions and of testers than the previous studies. The reports of the subjects regarding their sensations are similar to those reported by other authors29: discomfort or stretching sensation on anterior and radial aspects of the forearm, on the radial side of the hand and on I-IV fingers, and pins and needles in the hand. The mean ranges of elbow extension in asymptomatic subjects for OP and SP (155.0° ± 13.8° and 164.0° ± 9.3°) are similar to the ranges measured by Coppieters et al18 on ULNT1 with wrist extension under laboratory conditions (149.0° ± 22.8° and 159.7° ± 17.3°, respectively). Moreover, OP scores compared with SP, and R1 scores comparedwith R2, occurred about 10° earlier in the range.
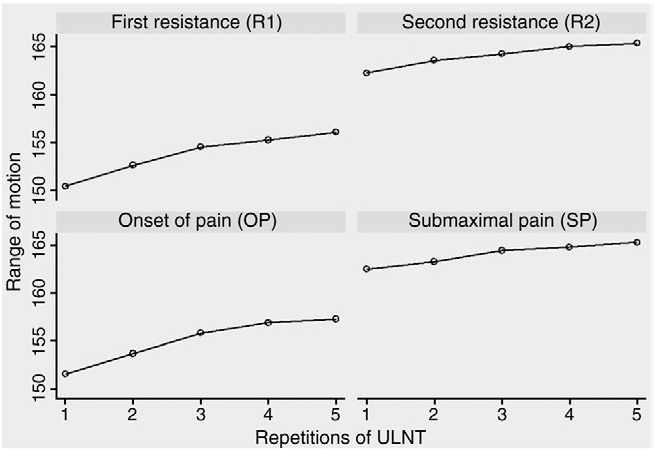
Fig 3. The effect of 5 repetitions on the elbow range (mean of 5 repetitions for all observers).
R1 is probably muscular in origin. Many authors have investigated this issue.30-34 In contrast, it is possible that R2 involves the nervous system more directly, even if not exclusively; however, the explanation of howtissues generate resistance is beyond the scope of this article. The intra- and intertester reliabilities were higher for subject parameters (OP, SP) in comparison to examiner parameters (R1, R2), a finding that is not unexpected given that assessing resistance is related to a perception by the examiner and, therefore, greater variability in results would be normally anticipated. However, it is interesting that the reliabilities for SP and R2 were stronger than those for OP and R1. The intratester reliability for OP and SP as calculated in this study is in the good range, even if not comparable to the findings in the “excellent” range for intratester/intrasession reliability of the same test noted by van der Heide et al17 and by Coppieters et al18 on asymptomatic subjects under laboratory conditions. We cannot compare our findings on the intratester reliability for OP, SP, R1, and R2 because we were unable to locate any similar studies in the peer-reviewed literature using asymptomatic subjects tested under clinical conditions. The experimental setting and the procedure for performing the ULNT1 that we used were established to minimize sources of errors as much as possible, but also generally remain true to the main characteristics of a clinical setting, in which this test is commonly used. The data relative to the intratester reliability are comparable to several studies published in the broader manual therapy literature that in general show good to excellent intraexaminer reliability for passive tests (such as R1 and R2 in our case) and for provocative tests (such as OP and SP). Regarding the intertester reliability for OP and SP in asymptomatic subjects, the results of this study suggest that our intertester reliability was not as strong as what other investigators have found16,18; but these studies might not have used comparable data. The main difference between other investigations and our study was the presence of external devices to maintain or control the head and the shoulder girdle in neutral position.
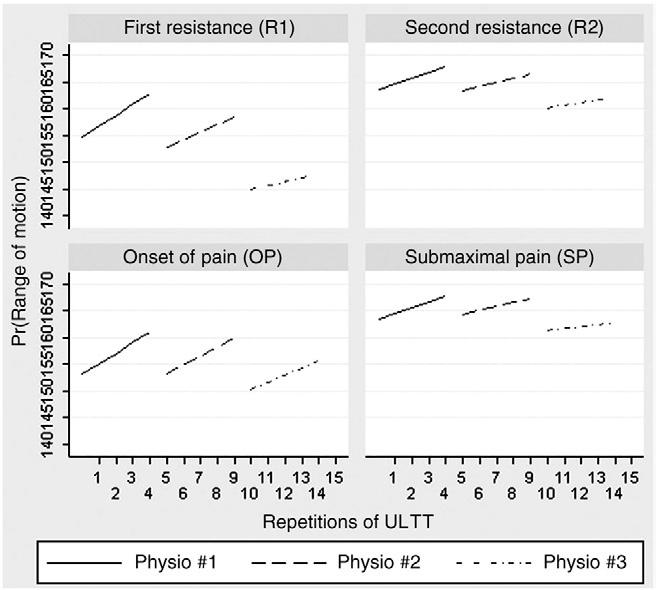
Fig 4. The effect of 15 repetitions on the elbow range (mean of 5 repetitions for each observer).
In a clinical setting, these positions could slightly vary between examiners, which might modify the tension of cervical roots, influence the range of other components of the ULNT1, and consequently alter the final result. Higher intra- than interexaminer reliability was found also by Reisch et al35 in their study of the ULNT2–median bias. She observed good to excellent intratester reliability (ICCs ranging from 0.88 to 0.94) and poor intertester reliability (ICC = 0.33). We must consider that administration of both ULNT1 and ULNT2 introduces each component of the test in successive phases and, thus, the tension applied during any one component in one phase can influence the next one.36 As a consequence, increased variability between testers is highly likely. We found that both intra- and intertester reliabilities appear to be slightly better for more expert physiotherapists. The reason for this observation is quite obvious and not uncommon in the manual therapy literature.14,37,38 Our impression is that investigations of reliability published more recently in the literature appear to prefer using only experienced testers. Finally, we found a definite effect of repetitions of each ULNT1 on the parameters OP, SP, R1, and R2, similar to the findings Coppieters et al.18 Although the analyses of Coppieters et al approached but did not reach statistical significance, we found a similar trend in asymptomatic subjects; and in our study, with a greater number of repetitions, the findings on both subjects and examiners reached statistical significance (P = .00). This result, in line with other similar findings,39,40 strongly suggests a mobilizing effect and a consequent progressively reduced resistance in the muscular, connective, cutaneous, vascular, and nervous tissues.(41) The progressive increase of the ROM during the 5 repetitions seems to disappear between a set of the ULNT1 and the next one. One possible explanation is that the effect was transient and that the rest of about 1 minute between an examiner and the next was enough to bring the tension of the tissues in a condition similar to that of departure. This magnitude of this increase in ROM is variable between different subjects and is inversely proportional to the ROM measured during the first repetition. Although outside the scope of the present study, the apparent effect of repetition on increasing elbow range in asymptomatic subjects has implications for both research methods and clinical practice and warrants further investigation.
Limitations
The main limitations of our study are related to the small sample of subjects, which does not reflect the clinical population, and to the limited sample of testers. Finally, future investigations will need to address the reliability, validity, the effect of the repetitions of the test, and the effect of the following rest in symptomatic individuals using different amount and set of this technique, so that we might better understand the biomechanical and clinical implication of neurodynamic testing for both evaluation and treatment.
CONCLUSIONS
Our finding indicated good intratester reliability of ULNT1 for all 4 parameters we investigated (OP, SP, R1, and R2) using asymptomatic subjects. Intertester reliability was observed to be fair to good considering the first repetition, and good considering the main of 5 repetitions. Our results align with other studies on the reliability of manual therapy tests, which generally show better intrathan intertester reliability, and are also consistent with previous studies on the particular test (ULNT1) we used. The positive effect of several repetitions may indicate the use of repeated ULNT1 as a treatment to mobilize tissues, but additional studies are needed on this topic.
Practical Applications
- The ULNT1 could be reliably used to compare the findings of several sessions by the same physiotherapist, but it could be less reliable for comparing the findings between different physiotherapists.
- This study suggests a direct correlation between intertester reliability and physiotherapists’experience.
- The effect of the repetitions of the ULNT1 is a progressive improvement of range from the first to the final repetition.
FUNDING SOURCES AND POTENTIALCONFLICTS OF INTEREST
No funding sources or conflicts of interest were reported for this study. Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
REFERENCES
- Jepsen JR, Laursen LH, Hagert CG, Kreiner S, Larsen AI. Diagnostic accuracy of the neurological upper limb examination I: inter-rater reproducibility of selected findings and patterns. BMC Neurol 2006;6:8.
- Shacklock M. Clinical neurodynamics: a new system of neuromusculoskeletal treatment. Oxford: Elsevier; 2005.
- Hall TM, Elvey RL. Nerve trunk pain: physical diagnosis and treatment. Man Ther 1999;4:63-73.
- Nee B, Butler D. Management of peripheral neuropathic pain: integrating neurobiology, neurodynamic and clinical evidence. Phys Ther Sport 2006:36-49.
- Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine 2003;28:52-62.
- Butler DS. The sensitive nervous system. Adelaide. Unley: Noigroup Publication; 2000.
- Elvey RL, Hall T. Neural tissue evaluation and treatment. In: Donatelli RA, editor. Physical therapy of the shoulder, 3rd edNew York: Churchill Livingstone; 1997. p. 131-52.
- Shacklock M. Improving application of neurodynamic (neural tension) testing and treatments: a message to researchers and clinician. Man Ther 2005;10:175-9.
- Shacklock M. Neurodynamics. Physiotherapy 1995;81:1.
- Kleinrensink G, Stoeckart R, Mulder PGH, Hoek G, Broek Th, Vleeming A, Snijders CJ. Upper limb tension tests as tools in the diagnosis of nerve and plexus lesions. Anatomical and biomechanical aspects. Clin Biomech 2000;15:9-14.
- Kleinrensink G, Stoeckart R, Vleeming A, Snijders C, Mulder P. Mechanical tension in the median nerve. The effects of joint positions. Clin Biomech 1995;10:240-4.
- Wright TW, Glowczewskie F, Wheeler D, Miller G, Cowin D. Excursion and strain of the median nerve. J Bone Joint Surg
Am 1996;78A:1897-903. - Rubinstein SM, Van Tulder M. A best-evidence review of diagnostic procedures for neck and low-back pain. Best Pract
Res Clin Rheumatol 2008;22:471-82. - Hines T, Noakes R, Manners B. The upper limb tension test: inter-tester reliability for assessing the onset of passive
resistance R 1. J Manipulative Physiol Ther 1993:95-8. - Maitland GD. Vertebral manipulation. 4th ed. London: Butterworths; 1977.
- Byng J. Overuse syndromes of the upper limb and the upper limb tension test: a comparison between patients, asymptomatic keyboard workers and asymptomatic non-keyboard workers. Man Ther 1997;2:157-64.
- Heide van der B, Allison GT, Zusman M. Pain and muscular responses to a neural tissue provocation test in the upper limb. Man Ther 2001;6:154-62.
- Coppieters M, Stappaerts K, Janssens K, Jull G. Reliability of detecting ‘onset of pain’ and ‘submaximal pain’ during neuralprovocation testing for the upper quadrant. Physiother Res Int2002;7:146-56.
- Chesworth BM, MacDermid JC, Roth JH, Patterson SD. Movement diagram and qend-feelq reliability when measuring passive lateral rotation of the shoulder in patients with shoulder pathology. Phys Ther 1998;78:593-601.
- Piriyaprasarth P, Morris M, Winter A, Bialocerkowski A. The reliability of knee joint position testing using electrogoniometry. Musculoskelet Disord 2008;9:6.
- Rowe PJ, Myles CM, Hillmann SJ, Hazlewood ME. Validation of flexible electrogoniometry as a measure of joint kinematics. Physiotherapy 2001;87:479-88.
- Walker C. Movement of the knee in osteoarthritis: the use of electrogoniometry to assess function. J Bone Joint Surg 2001; 83-B:195-8.
- Szuic P, Lewandowski J, Marecki B. Verification of selected anatomical landmarks used as reference points for universal goniometer positioning during knee joint mobility range measurements. Med Sci Monit 2000;7:312-5.
- Rome K, Cowieson FA. Reliability study of the universal goniometer, fluid goniometer, and electrogoniometer for the measurement of ankle dorsiflexion. Foot Ankle Int 1996;17: 28-32
- Ball P, Johnson G. Reliability of hindfoot goniometry when using a flexible electrogoniometer. Clin Biomech 1993;8: 13-9.
- Rawes ML, Richardson JB, Dias JJ. A new technique for the assessment of wrist movement using a biaxial flexible electrogoniometer. J Hand Surg 1996;21:600-3.
- Ojima H, Miyake S, Kumashiro M, Togami H, Meng S, Suzuki K. Dynamic analysis of wrist circumduction: a new application of the biaxial flexible electrogoniometer. Clin Biomech 1991;6:221-9.
- Goodwin J, Clark C, Deakes J, Burdon D, Lawrence C. Clinical methods of goniometry: a comparative study. Disabil Rehabil 1992;14:10-5.
- Selvaratnam PJ, Matyas TA, Glasgow EF. Noninvasive discrimination of brachial plexus involvement in upper limb pain. Spine 1994;19:26-33.
- Coppieters MW, Stappaerts KH, Staes FF, Everaert DG. Shoulder girdle elevation during neurodynamic testing: an assessable sign? Man Ther 2001;6:88-96.
- Coppieters MW, Stappaerts KH, Wouters LL, Janssens K. Aberrant protective force generation during neural provocation testing and the effect of treatment in patients with neurogenic cervicobrachial pain. J Manipulative Physiol Ther 2003:99-106.
- Costantini M, Tunks K, Wyatt C, Zettel H, MacDermid JC. Age and upper limb tension testing affects current perception thresholds. J Hand Ther 2006;19:307-16.
- Jaberzadeh S, Scutter S, Nazeran H. Mechanosensitivity of the median nerve and mechanically produced motor response during Upper Limb Neurodynamic Test 1. Physiotherapy 2005;91:94-100.
- Saranga J, Green A, Lewis J, Worsfold C. Effect of a cervical lateral glide on the upper limb neurodynamic Test 1. Physiotherapy 2003;89:678-81.
- Reisch R, Williams K, Nee RJ, Rutt RA. ULNT2–median nerve bias: examiner reliability and sensory responses in asymptomatic subjects. J Manipulative Physiol Ther 2005;13: 44-55.
- Coppieters MW, Butler DS. Do “sliders” slide and “tensioners” tension? An analysis of neurodynamic techniques and considerations regarding their application. Man Ther 2008;13:213-21.
- Johnston WL, Allan BR, Hendra JL, Neff DR, Rosen ME, Thomas SC. Interexaminer study of palpation in detecting location of spinal segmental dysfunction. J am Osteopath Assoc 1993;82:839-45.
- Muellner T, Bugge W, Johansen S, Holtan C, Engebretsen L. Inter- and intratester comparison of the Rolimeter knee tester: effect of tester’s experience and the examination technique. Knee Surg Sports Traumatol Arthrosc 2001;9: 302-6.
- Fidel C, Martin E, Dankaerts W, Allison G, Hall T. Cervical spine sensitizing maneuvers during the slump test. J Manipulative Physiol Ther 1996;4:16-21.
- Herrington L. Effect of different neurodynamic mobilization techniques on knee extension range of motion in the slump position. J Manipulative Physiol Ther 2006;14: 101-7.
- Walsh M. Upper limb neural tension testing and mobilization. Fact, fiction, and a practical approach. J Hand Ther 2005;18: 241-58.

